Being told a tooth needs a root canal can feel alarming, but modern endodontic treatment is designed to be predictable, comfortable, and focused on saving your natural tooth. Root canal therapy removes diseased tissue from inside a tooth, relieves pain, and restores function so you can eat, speak, and smile with confidence.
At the office of Brown Family Dentistry Group, we combine careful diagnosis with gentle techniques and updated technology to deliver conservative care that preserves as much of your tooth as possible. Our team prioritizes your comfort and clear communication so you understand each step of treatment and the reasons behind our recommendations.
When the inner tissues of a tooth become infected or irreversibly damaged, a root canal often provides the best chance to retain that tooth rather than extract it. Preserving a natural tooth maintains chewing efficiency, helps prevent adjacent teeth from shifting, and supports long-term oral health in ways replacements cannot always match.
Root canal procedures have a high long-term success rate when performed and followed by proper restoration. The goal is to remove infection, seal the internal anatomy, and protect the remaining structure so the tooth can continue to function for many years.
Choosing to save a tooth with root canal therapy also keeps treatment less invasive overall. By stabilizing the tooth now, you reduce the likelihood of more involved procedures later and help maintain your natural bite and jaw alignment.

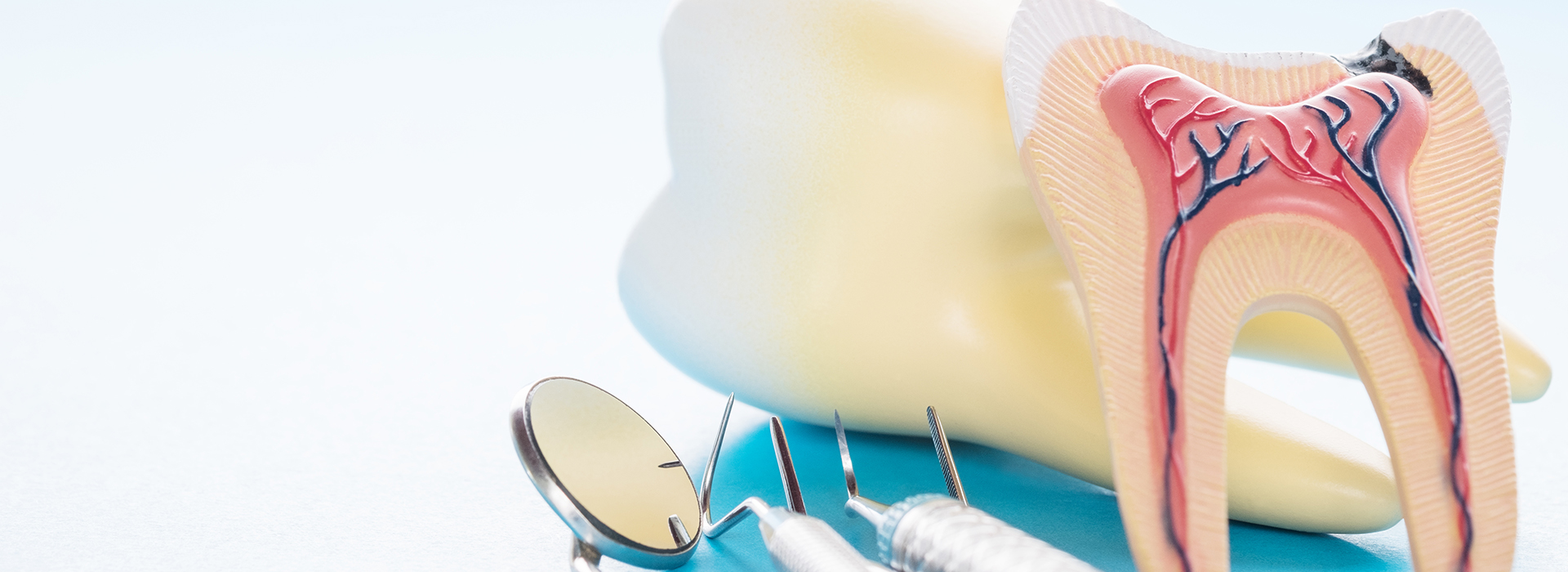
Each tooth contains an inner chamber filled with soft tissue — the dental pulp — that includes nerves and blood vessels. This tissue supports the tooth’s development and can signal when something is wrong by producing sensations such as pain or sensitivity.
Symptoms range from subtle changes to intense discomfort. Sometimes a tooth shows no pain at all, yet X-rays or clinical exams reveal infection around the root tip. That’s why attentive examination and imaging are important whenever you notice any change in a tooth’s appearance, sensation, or stability.
Understanding common warning signs helps you seek care earlier. Left untreated, an infected tooth can lead to increasing pain, bone loss around the root, swelling, and a higher risk of systemic complications. Prompt assessment helps preserve options and improves outcomes.
Below are several frequently observed indicators that a tooth may require root canal treatment:
A persistent toothache that lingers or wakes you at night often points to inflammation or infection inside the tooth. Pain that does not respond to typical measures should be evaluated to determine whether endodontic therapy is needed.
Sharp, lingering sensitivity to hot or cold foods and beverages can indicate the pulp is irritated or compromised. When sensitivity is severe or prolonged, it warrants a clinical exam and appropriate imaging.
Discomfort when chewing or when the tooth is tapped often reflects involvement of the internal tissues or an advancing infection that affects surrounding structures.
A tooth that becomes discolored after trauma or over time can indicate internal changes such as tissue death. Discoloration is a sign to have the tooth examined even if pain is absent.
A broken tooth can expose the inner tissues and allow bacteria to enter, creating a pathway for infection. Even small fractures can compromise the pulp and lead to deeper problems if untreated.
Swelling, tenderness, or the presence of drainage are classic signs of an active infection. These findings require timely attention to prevent spread and to manage symptoms effectively.
When the supporting bone or periodontal tissues are affected by infection, a tooth may feel loose. Treating the underlying cause can often stabilize the tooth and promote healing of surrounding tissues.

Some teeth announce trouble through pain or visible changes; others reveal problems only on X-rays taken during routine exams. In both cases, earlier intervention preserves more tooth structure, reduces the chance of complications, and often makes treatment simpler and more comfortable.
Delaying care allows infection to progress, which can increase the extent of treatment required and the risk to nearby tissues. Addressing issues promptly helps protect the rest of your mouth and supports overall oral health.
When our team identifies a tooth that may benefit from root canal therapy, we review the findings, outline the treatment steps, and answer your questions so you can make an informed decision with confidence.
Modern root canal therapy is designed for predictability and patient comfort. Treatment begins with a careful evaluation, use of local anesthesia to numb the area, and isolation of the tooth so the internal work can be done precisely and cleanly.
The procedure typically involves removing the diseased pulp tissue, disinfecting and shaping the internal canals, and placing a biocompatible filling material to seal the space. Some cases can be completed in a single visit; others may need additional appointments depending on the tooth’s anatomy and the presence of infection.
For patients who feel anxious about dental procedures, dental sedation and other comfort options are available and discussed in advance. After the internal therapy is finished, the tooth is temporarily restored and scheduled for a final restoration to rebuild strength and function.

Recovery after a root canal is generally straightforward. You may experience numbness until the anesthetic wears off, followed by mild soreness as surrounding tissues settle. Over-the-counter pain relievers usually manage any discomfort, and our team will provide specific aftercare instructions tailored to your needs.
If antibiotics are prescribed for an active infection, it’s important to complete the full course exactly as directed. Proper medication use supports healing and reduces the chance of lingering problems.
Although the internal infection is addressed during root canal therapy, the treated tooth remains more vulnerable than an untouched tooth until it is fully restored. A final crown or appropriate permanent restoration strengthens the tooth and helps protect it from fracture or recontamination.
After your appointment, avoid chewing until sensation returns to reduce the risk of accidentally biting your cheek, lip, or tongue. Take care with hot drinks until feeling is fully restored.
Mild soreness is common for a few days. Follow the recommended pain-management plan, rest as needed, and contact the office if pain intensifies or does not improve as expected.
If antibiotics are part of your treatment, taking them exactly as prescribed helps resolve infection and supports predictable healing.
Limit chewing on the side of the treated tooth until the permanent restoration is placed. Avoid hard or sticky foods that could stress the temporary filling.
Continue routine brushing and flossing to support healing and overall oral health. Clean, healthy tissues help a treated tooth remain stable in the long term.
Follow up with your dentist to arrange placement of a permanent crown or restoration. Completing this final phase protects the tooth and restores full function.
With careful treatment, timely restoration, and routine dental care, a tooth that has undergone root canal therapy can remain functional and comfortable for many years. If you have questions about symptoms you’re experiencing or want to learn whether root canal treatment is the right option, please contact us for more information and guidance.
A root canal procedure is the best way to save a tooth that has been damaged by decay or injury and preserve your natural smile. The alternative is an extraction and treatment to replace the tooth. While at times a tooth is non-restorable and an extraction is the only option, when possible, it’s best to try and save your natural tooth. With proper care, a tooth with root canal therapy can serve your smile well for many years to come.
Despite lingering myths from before the age of modern dental anesthesia and technology, having a root canal procedure today is as routine and comfortable as visiting the dentist for a filling. While the procedure is performed under local anesthesia with your tooth completely numbed, we can also discuss options in dental sedation.
Whether the symptoms of a dental infection subside after a course of antibiotics, a draining abscess provides you with some temporary pain relief, or a tooth with radiographic evidence of pathology has not yet developed symptoms, it’s essential, before an infection worsens or occurs, to have a root canal procedure performed. In this way, the tooth can be disinfected, filled, and sealed to protect your health and avoid further problems.
If you have sustained a dental injury, have a toothache, jaw pain, swelling, or are experiencing any other unusual and uncomfortable oral symptoms, contact our office immediately for care. Dental problems that have not been evaluated and treated can significantly worsen, producing more severe damage and consequences for the involved teeth, your oral health, and even your overall wellbeing. Once you get in touch with our office, our friendly and compassionate office team will get you in for care at your earliest convenience.
While some root canal procedures can be completed in one visit, others may involve 2 or 3 appointments. How long it takes depends on various factors, including active infection, the number of canals in the tooth, and the tooth’s location or anatomy.
With a success rate that exceeds 95%, root canal therapy remains the most effective procedure to save a tooth in which the inner vital tissues have been damaged. However, as with all healthcare procedures, there are a small percentage of cases where the teeth become symptomatic a second time. The good news is that many of these teeth can still be saved with root canal retreatment or a minor surgical procedure known as an apicoectomy.
The best ways to maintain a tooth with root canal therapy are to get the proper restoration required to rebuild and protect the tooth, maintain proper oral hygiene, and schedule appointments for routine dental checkups and care.
Saving a tooth with root canal therapy is a wise investment that, in the long run, is typically less costly and invasive than having the tooth extracted and replaced with a fixed bridge or implant. As far as the exact cost of care, it can vary depending on which tooth is being treated. Many dental insurance plans provide coverage for root canal therapy. At the office of Brown Family Dentistry Group, we do our best to optimize your dental benefits and minimize your out-of-pocket expenses. Our staff will answer all your questions about the cost of care and discuss all your payment options.
At the office of Brown Family Dentistry Group, we use the latest technology and most effective methods of care to provide precise and gentle care. Our reputation for excellence is based upon a consistent record of achieving successful treatment outcomes while providing prompt, stress-free, and convenient treatment for every type of dental need.
A root canal is a dental procedure that removes infected or irreversibly damaged tissue from inside a tooth and seals the canals to prevent reinfection. The treatment preserves the remaining tooth structure and eliminates the source of pain caused by inflammation or infection of the pulp. When successful, a root canal allows patients to keep their natural tooth and maintain normal chewing and appearance.
Root canal therapy is recommended when the dental pulp has been compromised by deep decay, trauma, or repeated dental procedures that lead to inflammation or infection. Early treatment prevents the spread of infection to the surrounding bone and adjacent teeth and reduces the likelihood of more complex treatment later. At Brown Family Dentistry Group, we emphasize timely diagnosis and gentle, evidence-based care to help patients retain healthy, natural teeth whenever feasible.
Common signs that a tooth may need root canal therapy include persistent or severe tooth pain, prolonged sensitivity to hot or cold, pain when biting or touching the tooth, visible discoloration, or swelling of the gums near the affected tooth. Some teeth with significant internal damage may not cause noticeable symptoms but can show radiographic signs of infection during a comprehensive exam. Any combination of these findings warrants prompt evaluation by your dentist.
Diagnosis typically involves a clinical exam, vital testing of the tooth, and diagnostic imaging such as digital X-rays to assess the extent of pulp involvement and any bone changes around the root tip. Your dentist will rule out other sources of pain, evaluate the tooth's restorability, and explain recommended options. Timely assessment helps prevent progression of infection and improves the likelihood of a predictable outcome.
Modern root canal procedures are performed under local anesthesia and are generally no more uncomfortable than having a routine dental filling. Advances in techniques and instruments, together with effective pain control protocols, allow most patients to undergo treatment without significant discomfort during the appointment. For those with dental anxiety, additional sedation options can further improve comfort and reduce stress.
It is common to experience mild to moderate tenderness or soreness for a few days after the procedure as surrounding tissues heal, but this is typically manageable with over-the-counter pain relievers or prescribed medications when indicated. If pain increases, persists beyond a few days, or is accompanied by swelling or fever, contact the dental office promptly for evaluation and care. Close follow-up ensures any complications are identified and treated early.
During a non-surgical root canal, the dentist isolates the tooth with a rubber dam, creates a small access opening, and removes the diseased pulp using specialized instruments and irrigation solutions to disinfect the canals. After cleaning and shaping the internal spaces, the canals are dried and filled with a biocompatible material to seal them against bacteria. The access opening is then sealed with a temporary or permanent filling to protect the tooth.
Some teeth can be completed in a single visit while others may require two or more appointments depending on anatomy, the presence of infection, or additional restorative needs. Throughout every step, strict infection-control protocols and modern instruments support a precise and predictable outcome. Your dentist will explain each phase of treatment and any post-procedure instructions to support healing.
Most patients recover quickly after root canal therapy and can return to normal activities within a day, though mild soreness or sensitivity around the treated tooth may persist for several days. Over-the-counter anti-inflammatory medications usually control discomfort, and cold compresses can help reduce swelling when needed. Any numbness from local anesthesia typically resolves within a few hours.
It is important to follow your dentist's recommendations for restoration of the tooth, as a definitive crown or suitable restoration strengthens the tooth and reduces the risk of fracture. If antibiotics or additional medications are prescribed, take them exactly as directed and attend any scheduled follow-up visits. If symptoms worsen or new concerns arise, contact Brown Family Dentistry Group for prompt evaluation and guidance.
Yes, root canal therapy is specifically designed to save a tooth that would otherwise require extraction due to irreversibly damaged or infected pulp. By removing the diseased tissue, disinfecting the canals, and sealing the system, the tooth can remain functional and stable for many years. Preserving the natural tooth helps maintain proper chewing function, jawbone support, and the alignment of surrounding teeth.
The long-term success of a treated tooth depends on factors such as the quality of the root canal filling, proper restoration, and the patient’s oral hygiene habits. Placing a crown or appropriate permanent restoration often provides protection against fracture and recontamination. Regular dental checkups and good home care support the longevity of root canal treated teeth.
Alternatives to root canal treatment include extraction of the affected tooth followed by replacement options such as dental implants, bridges, or removable prostheses, or conservative monitoring in select cases where the pulp may recover. For immature teeth with reversible pulpitis, a less invasive pulp capping or pulpotomy may be considered to preserve vitality. Each alternative carries its own indications, benefits, and long-term considerations.
Your dentist will review the most appropriate options based on the condition of the tooth, overall oral health, and your treatment goals. In many cases, saving the natural tooth with root canal therapy is the preferred and most conservative approach. Shared decision-making ensures you understand the trade-offs and expected outcomes of each pathway.
Many teeth that undergo root canal therapy benefit from a crown or other full-coverage restoration to protect the remaining tooth structure and restore function. Teeth that have lost substantial tooth material, those in high-stress areas, or posterior teeth that do most of the chewing are particularly good candidates for crowns to reduce the risk of fracture. A proper restoration helps seal the tooth against bacteria and supports long-term success.
The timing of a crown varies; some patients receive a permanent restoration shortly after root canal therapy, while others may have a temporary filling until final restoration is completed. Your dentist will evaluate the tooth's structural needs and recommend the ideal restoration type and timeline to help you resume normal chewing with confidence.
Good oral hygiene is essential after root canal therapy: continue to brush twice daily with fluoride toothpaste, floss daily, and maintain routine dental cleanings and examinations. Avoid hard, sticky, or excessively chewy foods on the treated tooth until a permanent restoration is placed to reduce the risk of fracture. If you clench or grind your teeth, discuss protective options such as a night guard to prevent excessive forces on the restored tooth.
Attend scheduled follow-up visits so your dentist can confirm healing and assess the restoration, and report any new or worsening symptoms promptly. Maintaining overall oral health, addressing periodontal concerns, and promptly repairing any restorative issues will all contribute to the long-term function of a root canal treated tooth. Preventive care and early attention to changes help ensure the tooth remains serviceable for many years.
If you experience increasing pain, persistent swelling, drainage, fever, or any new symptoms after a root canal, contact your dental office promptly for evaluation. Manage acute discomfort with recommended medications and cold compresses while you arrange for professional assessment, and avoid placing pressure on the treated tooth. Early attention allows your dentist to determine whether further treatment, such as retreatment, adjustment of the restoration, or management of an infection, is needed.
Minor soreness in the days following treatment can be expected, but escalating symptoms or signs of spreading infection require urgent care. Keep records of medication instructions and follow-up appointments, and notify the practice if prescribed antibiotics or pain control measures are not producing improvement. Timely communication and follow-up care help ensure the best possible outcome.

Ready to schedule your next dental appointment or have questions about our services?
At Brown Family Dentistry Group, connecting with us is easy! Our friendly staff is here to assist you with appointment scheduling, answer questions about treatment options, and address any concerns. Call, email, or use our quick online contact form—whichever works best for you. Take the first step toward a healthier, more confident smile today and experience the difference personalized dental care can make.